Delaware to Expand Statewide Telehealth Program | ALA Annual 2022
Following a successful pilot test at Delaware’s Seaford, Laurel, and Milford libraries, the Delaware Division of Libraries (DDL) is preparing to roll out a new, comprehensive telehealth program to nine additional locations throughout the state by the end of 2022. The program was discussed in depth during “The First Statewide Library-Led Telehealth Initiative in the First State” presentation on June 26 at the American Library Association’s 2022 Annual Conference and Exhibition in Washington, DC.
 Following a successful pilot test at Delaware’s Seaford, Laurel, and Milford libraries, the Delaware Division of Libraries (DDL) is preparing to roll out a new, comprehensive telehealth program to nine additional locations throughout the state by the end of 2022. The program was discussed in depth during “The First Statewide Library-Led Telehealth Initiative in the First State” presentation on June 26 at the American Library Association’s 2022 Annual Conference and Exhibition in Washington, DC.
Following a successful pilot test at Delaware’s Seaford, Laurel, and Milford libraries, the Delaware Division of Libraries (DDL) is preparing to roll out a new, comprehensive telehealth program to nine additional locations throughout the state by the end of 2022. The program was discussed in depth during “The First Statewide Library-Led Telehealth Initiative in the First State” presentation on June 26 at the American Library Association’s 2022 Annual Conference and Exhibition in Washington, DC.
Public libraries have several qualities that make them good hosts for telehealth services, explained presenter Nick Martin, emerging technology consultant, Delaware Libraries. While many people in rural areas don’t have convenient access to clinics or other medical facilities, almost 100 percent of the U.S. population lives within five miles of a library branch, he said, citing a report by the Center for Urban Research at the City University of New York’s Graduate Center. Similarly, in a 2015 public poll by the Pew Research Center, 87 percent of respondents said that libraries are useful for seeking health information, he said. “Prior to telehealth programs, that was researching…on the internet and talking to [library] staff, or attending programs with community partners,” he said. “But we know the community sees the library as a place to access this information. You couple that with the health literacy disparities that exist in the country right now…. It’s estimated about 36 percent of adults in the U.S. have low health literacy, with disproportionate rates affecting lower income Americans eligible for Medicaid.”
In addition, Martin said that about 10 percent of Delaware residents do not own a computing device, and 16 percent of households do not have broadband internet. “The pilot program was in the most southern, rural part of our state, where those percentages are even higher,” he said.
Once the need for these programs was established, Martin said that “the next step for me, in 2019, was determining how to become a subject matter expert in telehealth.” He took a 15-week course at the University of Delaware that covered technology evaluation, business and operational considerations, regulations, ethics, patient privacy, and more to earn a Certified Advanced Telehealth Coordinator certificate. (Other credentialing options include a Telehealth Facilitator Certificate through Thomas Jefferson University earned through a five-week course, and a Telehealth Coordinator Certificate through the National School of Applied Telehealth, which is earned through a 3–5 hour online course.) “Luckily, there are a lot of programs out there now that aren’t as long, or as expensive” as the semester-long course, he said.
PARTNERING WITH EXPERTS
Martin advised that libraries building a telehealth program should develop partnerships with hospitals, clinics, and/or health organizations and defer to them on matters of policy and logistics. “Leave [that] part to the experts,” he said. “It’s important to understand where things are, but for our program, we rely on our healthcare partners and Medicaid providers to really inform us and stay up-to-date” with policies regarding telehealth.
For DDL, those partners became healthcare systems ChristianaCare, Beebe Healthcare, and Nemours Children’s Health; health-related nonprofits JFS Delaware and the Sussex County Health Coalition; the state government’s Delaware Department of Health and Social Services, Division of Public Health (DDHSS); federally qualified health center La Red; behavioral health organizations Delaware Guidance Services, Dover Behavioral Health System, Project THRIVE, and SUN Behavioral; insurance providers Highmark Delaware and AmeriHealth Caritas Delaware; the University of Delaware and the University of Virginia; local tech organization NERDiT Now for technical support; and to help get the word out about the new service, cultural institutions La Esperanza and the Haitian Coalition of Delaware.
In addition, “there is a pretty robust network of telehealth experts in the U.S. that have been doing this for decades,” Martin noted, suggesting that libraries join local and regional groups—in this case, the Delaware Telehealth Coalition and the Mid-Atlantic Telehealth Resource Center—as well as national networks such as the Global Partnership for TeleHealth, the National Consortium of Telehealth Resource Centers, the American Telemedicine Association (ATA), and HLTH. These organizations have “great resources, including courses to train people on telehealth and telepresenting,” he said. “ATA in particular is really great for up-to-date policy information.”
PICKING UP THE TELEHEALTH TAB
To fund a pilot test or a new program, “for me what worked was keeping it local [regarding charitable organizations] and leveraging COVID funding” for grants, Martin said. “There’s always a way that you can…intertwine telehealth in libraries” into an American Rescue Plan Act request for proposal. “If you want to explore more national opportunities…your [Network of the National Library of Medicine] region will typically have great opportunities, I would say in the $20,000 to $25,000 range, to launch a pilot program like this.”
Delaware’s pilot was funded by grants from Barclays US Consumer Bank, the Delaware Community Foundation, DDHSS, the Crystal Trust Foundation, Discover Bank, Highmark Blue Cross Blue Shield Delaware, the Longwood Foundation, and the Welfare Foundation. In addition, Congresswoman Lisa Blunt Rochester this week visited the Laurel library and announced that $275,000 in federal funding has been awarded to help DDL expand the program to new locations.
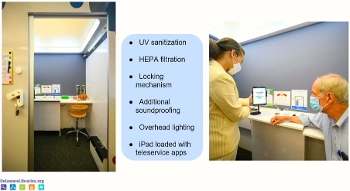
At each of the three pilot libraries, DDL installed soundproof booths developed by TalkBox that seat two to three people. The interiors are equipped with UV sanitation and HEPA filtration. In addition, at DDL’s request, the vendor included a locking mechanism, so that patients could be assured privacy during consultations, and library staff can lock the units when not in use. For consultations with DDL’s healthcare partners, patients are given an iPad loaded with teleservice apps and connected to the library’s broadband network. A staff “navigator” can also be present to help patients schedule appointments, assist with technology, or answer questions about the service.
DELIVERING QUALITY CARE
Now in operation a little over one year, telehealth services at the pilot libraries are operating at about 25 percent capacity, Martin estimated, citing the slow return of in-person visits to libraries following pandemic reopenings as one reason that many patrons may still be unaware of the program. To boost awareness, the library has begun using a combination of social media posts, radio ads, and direct outreach to local community leaders and groups. One of the most successful ways to promote the service, Martin said, has been inviting a nurse from their partner ChristianaCare to visit a branch to answer questions and offer blood pressure readings and basic screenings, and then explain that the branch’s new telehealth service is also available any time patients need to make an appointment. Also, during downtime, the libraries have been offering the booths for other uses that require privacy and a broadband connection, such as virtual job interviews.
In a pre-recorded video, Dr. Vishal Patel, primary care physician and associate medical director of ChristianaCare's Center for Virtual Health, addressed attendees, noting that “you may be wondering, ‘can you really provide high-quality care virtually?’ The answer is yes. We know that 95 percent of care can be done virtually,” including asking questions, reviewing a patient’s medical history, ordering and interpreting tests, collecting biometrics, conducting examinations that do not require physical contact, and observing patients following any treatments.
RELATED
ALREADY A SUBSCRIBER? LOG IN
We are currently offering this content for free. Sign up now to activate your personal profile, where you can save articles for future viewing







Add Comment :-
Comment Policy:
Comment should not be empty !!!